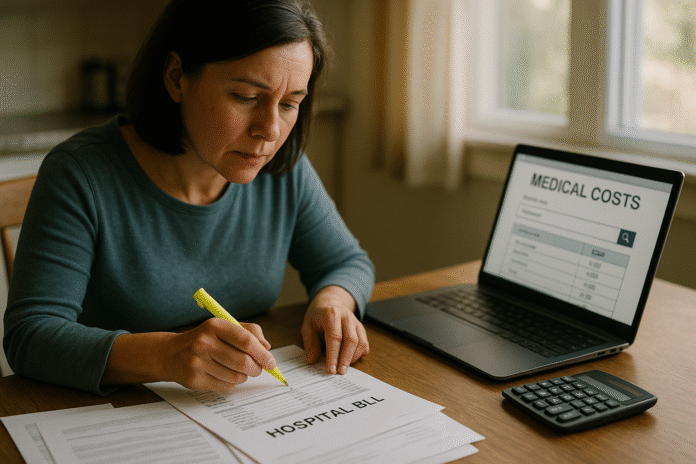
If you’re staring at a hospital or doctor bill that feels impossible, you’re not stuck with the first number you see. Negotiating Medical Bills means using your rights, correcting errors, comparing prices, and choosing a payment plan that fits your budget. In practice, it’s a mix of fact-checking, asking for help, and making an offer that’s anchored to real benchmarks. Quick answer: you can almost always lower a medical bill by requesting an itemized statement, verifying coding, appealing insurance mistakes, checking transparent prices/Medicare rates, applying for financial assistance, and negotiating a prompt-pay discount or payment plan. For fast action, work this mini-plan: itemized bill → compare to EOB → check codes → appeal insurer → price-check → ask for charity care → request prompt-pay → propose a number → set a 0% plan → use No Surprises Act rights if applicable → protect your credit → escalate with records.
This guide is educational and general, not medical, legal, or financial advice. U.S. rules are referenced; if you’re outside the U.S., check your local regulations.
1. Get an Itemized Bill and Match It to Your Explanation of Benefits (EOB)
Start by requesting an itemized bill from the provider and do not pay a summary statement. Itemization lists each service, date, quantity, and code so you can spot errors and duplicates. If you used insurance, wait for your Explanation of Benefits (EOB) from your health plan; it’s not a bill, but it shows what was charged, what your plan allowed, and what you may owe. Compare the EOB line-by-line with the itemized bill: dates of service, provider names, CPT/HCPCS codes, quantities, and modifiers should align. If the provider’s bill exceeds the plan’s allowed amount or includes services your EOB shows were disallowed or bundled, flag it in writing and ask for a corrected claim. The Centers for Medicare & Medicaid Services (CMS) explains that an EOB outlines provider charges, allowed charges, plan payment, and your share—and that an EOB is not a bill. Use it as your reconciliation sheet before negotiating.
1.1 How to do it
- Ask: “Please send an itemized statement with CPT/HCPCS and ICD codes for each charge.”
- Compare each charge on the bill to the EOB’s “allowed amount” and “paid by insurer.”
- Call the billing office to correct mismatches; follow up by email for a paper trail.
- If uninsured/self-pay, request a Good Faith Estimate (GFE) and keep it.
1.2 Mini-checklist
- Itemized bill received
- EOB received (if insured)
- Line-by-line match completed
- Written correction request sent
Bottom line: Treat the EOB as your benchmark and the itemized bill as the data source; both together reveal leverage points and fixable mistakes before you talk discounts.
2. Verify Coding, Dates, and Duplicates—Fix Obvious Errors First
The fastest savings often come from correcting mistakes. Coding drives price. CPT/HCPCS and ICD-10-CM codes tell insurers—and you—what was done and why. Errors like wrong laterality, upcoding (a higher-priced code than the service provided), unbundling (separating services that should be billed together), duplicate entries, or wrong dates can inflate a bill. Ask the provider’s coder or billing office to audit disputed lines; provide notes about what you actually received. You can also look up HCPCS definitions and confirm you’re not being billed for supplies or services that don’t apply. CMS maintains public information on HCPCS Level II (supplies, DME, certain services) and explains the coding system’s scope; their Physician Fee Schedule (PFS) pages also show how codes tie to payment for Medicare. While private insurance pays differently, these references help you question line items intelligently.
2.1 Common mistakes to look for
- Duplicate charges: same code/date billed twice.
- Wrong setting: inpatient vs. outpatient codes misapplied.
- Unbundled services: components billed separately when a single code should cover them.
- Supplies: generic “supply” codes that don’t match your visit.
2.2 Tools/Examples
- CMS HCPCS overview to understand supply/service codes.
- PFS lookup to confirm code descriptors and Medicare payment fields (as a reference point).
Bottom line: Fixing clear coding or duplication errors shrinks the target you need to negotiate—and makes the rest of the conversation about legitimate charges only. CMS
3. If You Used Insurance, Confirm Adjudication and Appeal Incorrect Denials
Before you negotiate with a provider, make sure your insurer processed the claim correctly. Start with the EOB remarks (coverage decisions, reasons for denial, or requests for more info). If a claim was denied, you usually have the right to an internal appeal—and often an external review—within deadlines set by your plan and state law. Use your EOB as the basis for your appeal, attach medical notes or prior-auth proofs, and cite network contracts when applicable. If your insurer isn’t responsive, you can escalate by filing a complaint with your state’s Department of Insurance; the National Association of Insurance Commissioners (NAIC) provides consumer guidance on complaints and how to route them in your state.
3.1 How to do it (short sequence)
- Call your insurer’s member services to clarify the denial code.
- Ask your provider to resubmit with correct codes or modifiers, if needed.
- File a written internal appeal by the deadline; keep receipts.
- If unresolved, pursue external review or file a DOI complaint. NAIC
3.2 Region notes
Appeal routes and timelines vary by state and plan type; your state DOI website lists your options and forms. Check your state’s portal (e.g., California’s consumer help page) for links to health-plan complaints and independent medical review programs. California Department of Insurance
Bottom line: A “denied” claim doesn’t mean you owe the full sticker price; fix the insurance processing first so your negotiation starts from the correct balance.
4. Price-Check Against Public Benchmarks and Hospital Transparency Files
To negotiate, anchor to real numbers. U.S. hospitals must publicly post standard charges in a machine-readable file and a consumer-friendly display for “shoppable services.” These include the gross charge, discounted cash price, and payer-specific negotiated rates. Use these to see how your line items compare. Pair this with free consumer tools like FAIR Health Consumer to see typical out-of-network prices in your ZIP code, and use the Medicare Physician Fee Schedule for a baseline—even though private rates differ, it’s a recognized reference. CMS has also strengthened transparency compliance in 2024–2025, including clearer access to machine-readable files.
4.1 How to do it
- Search your hospital’s website for “price transparency” or “standard charges.”
- Find the discounted cash price and payer-negotiated rate for your codes.
- Check FAIR Health Consumer for regional estimates to triangulate a fair target.
- Print/save the pages; you’ll cite them in your ask.
4.2 Numbers & guardrails
If your bill is far above the hospital’s own posted discounted cash price—or above what your insurer typically pays—that discrepancy is strong leverage to request a reduction to that posted level. CMS’ transparency rules are the basis for asking the billing office to honor their published figures.
Bottom line: Negotiations go better when you present their own published prices and regional benchmarks rather than debating abstracts.
5. Ask About Financial Assistance (Charity Care) If You Qualify
If you received care at a nonprofit hospital, U.S. tax law requires that facility to maintain a Financial Assistance Policy (FAP) and to make reasonable efforts to determine eligibility before taking extraordinary collection actions (like lawsuits or reporting to credit bureaus). FAPs typically set income thresholds (often expressed as a percentage of the Federal Poverty Level) for free or discounted care and detail how to apply. If you’re eligible, your charges must be limited below gross charges under the policy. Even if you’re over the threshold, hospitals sometimes offer hardship discounts. The IRS explains these requirements in Sections 501(r)(4), 501(r)(5), and 501(r)(6).
5.1 How to do it
- Ask: “Please send me your Financial Assistance Policy, plain-language summary, and application.”
- Provide proof of income, household size, and recent bills.
- Request a hold on collections while your application is under review (they should pause “extraordinary collection actions”).
5.2 Mini case
If your household income is within your hospital’s FAP threshold, a $4,000 outpatient bill could drop to a nominal amount or be fully waived under the policy’s discount schedule. Keep the approval letter—it’s the foundation for future adjustments.
Bottom line: If you might qualify, apply first—charity care can erase or sharply discount balances, reshaping the negotiation.
6. Request a Prompt-Pay or Cash Discount—Then Get It in Writing
Even if you don’t qualify for FAP, many providers offer prompt-pay or cash discounts for balances paid quickly. Use your transparency findings to set expectations (“Your posted cash price for CPT 70450 is $X; can you honor that if I pay this week?”). Ask the billing office to document any discount as an adjustment on the account, not just a verbal promise, and to send an updated statement. Patient-facing nonprofits and hospital financial counselors routinely point patients to prompt-pay discounts and affordable payment options; use their guidance and language.
6.1 Tips for the ask
- Lead with facts: transparency file numbers, FAIR Health ranges.
- Propose a round figure tied to those benchmarks.
- Ask to waive “facility” or “administrative” fees that aren’t on your estimate.
6.2 Close the loop
- Ask for a zero-balance letter or revised statement reflecting the reduction.
- Verify the provider won’t bill the remainder to insurance if you choose a self-pay discount.
Bottom line: A clear, anchored ask plus quick payment often wins a lower “cash” or “prompt-pay” amount—just memorialize it in writing.
7. Make a Reasonable Offer Anchored to Transparent Rates or Medicare Benchmarks
You’ll get further with an anchored offer than with “I can’t afford it.” Use three anchors: (1) the hospital’s discounted cash price for your code(s), (2) your plan’s typical allowed amount from the EOB, and (3) the Medicare rate from the PFS lookup. Medicare rates are not binding on private bills, but they’re a credible floor to frame reasonableness. Present a short memo: line items, published cash price, EOB allowed amount, your offer (e.g., 100% of discounted cash price, or a % above Medicare). Provide citations (screenshots/links) to the hospital’s transparency page and FAIR Health estimates.
7.1 Example offer (for one CPT code)
- Hospital discounted cash price: $480 (per transparency file).
- EOB allowed amount: $520 (payer X).
- Medicare national payment (non-facility): $210 (PFS lookup). CMS
- Offer: $500 if paid within 7 days, or $520 in 3 equal payments.
7.2 Why it works
You’re solving the provider’s cash-flow problem and using their own public numbers. It’s pragmatic, not adversarial.
Bottom line: Tie your offer to posted prices and a known reference (Medicare) to make “yes” the easy answer.
8. Set a 0% (or Low-Interest) Payment Plan You Can Actually Afford
If a lump sum isn’t realistic, ask for a no-interest payment plan with a payment you can sustain. Many hospitals will spread payments across 6–24 months interest-free; some use third-party vendors. Get terms in writing: monthly amount, term, interest (0% preferred), autopay authorization (optional), and a promise that the account won’t be sent to collections if you pay as agreed. Patient Advocate Foundation and hospital financial counselors routinely help patients find affordable payment plans—use their scripts if you’re uncomfortable asking. Patient Advocate Foundation
8.1 Mini-checklist
- Written plan with 0% interest (or lowest possible)
- Due date that aligns with your pay schedule
- Explicit “no collections if current” clause
- Autopay optional, not mandatory
8.2 Numeric example
On a $2,400 balance, ask for 0% over 24 months = $100/month. If they insist on interest, counter with a shorter term for a larger prompt-pay discount instead.
Bottom line: An affordable written plan prevents default and preserves your negotiating gains.
9. Use No Surprises Act Protections for Out-of-Network and “Surprise” Bills (and GFE for Self-Pay)
If you received emergency care or certain non-emergency ancillary services at an in-network facility, the No Surprises Act generally protects you from out-of-network balance bills; your cost-sharing is limited to in-network amounts. Providers must give disclosures about these protections, and there’s a federal Independent Dispute Resolution (IDR) process—between plan and provider—that keeps you out of the middle. For the uninsured/self-pay, you’re entitled to a Good Faith Estimate (GFE) in advance; if your final bill is $400+ above the GFE from a specific provider or facility, you can file a Patient-Provider Dispute Resolution (PPDR) to reduce the bill. As of August 2025, CMS maintains these rights and processes on its consumer pages.
9.1 How to act
- For emergency/out-of-network bills: cite the No Surprises Act and ask the provider to re-bill at in-network cost-sharing limits.
- For self-pay variances: if billed $400+ over your GFE, file a PPDR within 120 days of the bill date using CMS instructions.
9.2 Why it matters
These laws move negotiations from “please help” to “here’s the rule.” They’re your strongest leverage for surprise and self-pay scenarios.
Bottom line: Invoke NSA protections (insured) and GFE/PPDR rights (self-pay) to cap what you owe and dispute overcharges with legal backing.
10. Protect Your Credit and Handle Collections the Right Way
Medical debt rules have shifted. In April 2023, Equifax, Experian, and TransUnion removed medical collection debts under $500 from U.S. credit reports and stopped reporting paid medical collections; that change is still in place. In January 2025 the CFPB finalized a rule to remove medical bills from credit reports entirely, though a federal court vacated that rule in August 2025. Net: sub-$500 medical collections still shouldn’t appear, but broader removal may be on hold depending on ongoing litigation. If a collector contacts you, you have a 30-day window to request debt validation in writing; collectors must pause collection until they verify. Suing or threatening to sue on time-barred debt is prohibited under Regulation F. Use these rights to dispute errors, stop harassment, and avoid restarting the statute of limitations by mistake.
10.1 Steps if you’re contacted
- Send a validation request within 30 days; use CFPB model language.
- If inaccurate on your credit file, dispute with the bureau and furnish documentation.
- Ask the provider to pull back a newly assigned collection while you negotiate.
10.2 Guardrails
- Don’t make small “good-faith” payments on very old debts without advice—this can revive the statute in some states. Regulation F bars lawsuits on time-barred debt, but revival rules vary by state. Consumer Financial Protection Bureau
Bottom line: Use the 30-day validation window, avoid reviving time-barred debts, and leverage current reporting policies so medical bills don’t unfairly tank your credit.
11. Get Help from Patient Advocates and Nonprofit Resources—Strategically
You don’t have to go it alone. Patient Advocate Foundation (PAF) offers free case management to help with insurance denials, appeals, and unaffordable bills; they also operate disease-specific co-pay relief funds. Many hospitals employ patient financial counselors who can walk you through FAP applications and payment plans. Some communities partner with charities like Undue Medical Debt (formerly RIP Medical Debt), which buys and forgives bundled medical debts for qualifying residents—often automatically. Check state and local programs; many are using federal relief funds to erase eligible medical debt.
11.1 How to use help well
- Call PAF for free case management if an appeal or complex bill is stalled.
- Search local news or city/state sites for debt relief partnerships with Undue Medical Debt.
- Ask your hospital’s financial counselor to screen you for FAP, discounts, and 0% plans.
11.2 Fee caution
Be careful with for-profit “bill negotiation” services; clarify fees (flat vs. % of savings), success criteria, and refund policies before you sign.
Bottom line: Skilled advocates and targeted nonprofits can unlock discounts, approvals, and even full balance forgiveness you may not find alone.
12. Keep Records and Escalate When Needed (Compliance, Regulators, Complaints)
Documentation wins negotiations. Keep a dated log of calls, copies of every EOB/bill, transparency screenshots, and written agreements. If a provider or plan isn’t honoring the No Surprises Act, GFE/PPDR, or state rules, escalate with a formal complaint: CMS maintains consumer resources for medical-bill rights, and your state Department of Insurance handles plan complaints. For debt-collection abuses, file with the CFPB; you can also report unfair practices to the FTC. Clear, organized evidence accelerates resolution and helps regulators intervene.
12.1 Mini-checklist
- Timeline of events with dates
- Copies of EOBs, itemized bills, letters, and emails
- Screenshots/links to hospital price pages and FAIR Health results
- Complaint filed with the right agency, if needed
12.2 Synthesis
If you’ve followed the earlier steps, escalation isn’t a threat—it’s simply the next official step in enforcing the rules that already support your position.
Bottom line: Organized documentation plus the right escalation channel turns a lopsided bill dispute into a solvable compliance issue.
FAQs
1) What exactly counts as “Negotiating Medical Bills”?
It’s the process of reducing what you owe by correcting errors, applying financial assistance policies, and agreeing on a fair price or payment plan. You use documents (itemized bill, EOB, transparency files, GFEs) and laws (No Surprises Act, IRS 501(r), debt-collection rules) to support your ask. In short: verify, anchor, ask, and memorialize.
2) How do I know if my bill is “too high”?
Compare against three benchmarks: (1) your hospital’s discounted cash price for the same code(s), (2) your plan’s allowed amount on the EOB, and (3) Medicare rates from the Physician Fee Schedule. If your balance is above those anchors, you have a strong rationale to request a reduction.
3) I’m uninsured. Do I have any protection?
Yes. You’re entitled to a Good Faith Estimate before scheduled care, and if any provider’s bill is $400+ higher than that provider’s estimate, you can use a federal PPDR process to challenge and lower the bill (deadline applies). Keep copies of the GFE pages you receive.
4) The ER was out-of-network. Why am I still protected?
Emergency care and certain ancillary services at in-network facilities fall under the No Surprises Act, which limits your responsibility to in-network cost-sharing and prohibits balance billing in many scenarios. Dispute out-of-network balances by citing the law and asking for reprocessing at in-network amounts.
5) What if my hospital is nonprofit—do they have to help?
Nonprofit hospitals must publish a Financial Assistance Policy, limit charges for eligible patients, and make reasonable efforts before aggressive collections. Policies vary but often provide free or discounted care based on income. Ask for the FAP packet and apply if there’s any chance you qualify.
6) Can negotiating hurt my credit?
Negotiating itself won’t. Watch the calendar: ask the provider to pause collections while you resolve billing. Remember, debts under $500 should not appear as medical collections on your credit reports (policy since April 2023). A broader CFPB rule to remove medical bills entirely was finalized in 2025 but was vacated by a federal court in August 2025; watch for updates.
7) A collector is calling me—what should I do first?
Within 30 days, send a debt-validation letter (keep proof). The collector must stop collecting until they verify. If the debt is time-barred, they cannot sue or threaten to sue under Regulation F. Don’t make small payments on very old debts without understanding state “revival” rules.
8) Are there trustworthy tools to estimate fair prices?
Yes—start with your hospital’s transparency pages and FAIR Health Consumer to see regional estimates. For professional services, the Medicare Physician Fee Schedule lookup provides national and locality amounts, useful as a reference even for private insurance.
9) What if the provider refuses to budge?
Escalate politely: ask for a supervisor, then the billing manager or compliance office. File a written dispute, include your evidence, and copy your state Department of Insurance (if an insurance issue) or CFPB/FTC (if a collection issue). Organized documentation often triggers a second look. NAIC
10) How common is medical debt—and why is it so hard to pay?
Surveys consistently show a large share of U.S. adults carry medical debt; KFF found about 4 in 10 adults reported health-care debt, with higher rates among lower-income and uninsured people. High deductibles, denials, and out-of-network charges all play a role.
11) Will a hospital ever forgive my bill entirely?
Yes—through FAP charity care (if you qualify) or occasionally through philanthropic programs and city/state partnerships with groups like Undue Medical Debt, which buy and cancel eligible debts. Relief often happens automatically if you meet criteria, but it’s not guaranteed—ask the provider and watch local news.
12) What documents should I save for future care?
Keep a binder (or secure cloud folder) with: itemized bills, EOBs, GFEs, transparency screenshots, approval/denial letters, FAP decisions, payment-plan agreements, and any complaint filings. That file becomes your template for faster, easier negotiations next time.
Conclusion
Negotiating medical bills works because you’re not “arguing a price”—you’re restoring accuracy, applying written policies, and solving a real cash-flow problem for the provider. The playbook is straightforward: confirm the claim was processed correctly, correct coding issues, anchor to transparent prices and Medicare benchmarks, and ask for charity care, prompt-pay discounts, or a 0% payment plan. If it’s an out-of-network surprise, invoke the No Surprises Act; if you’re self-pay, use the Good Faith Estimate/PPDR pathway. Throughout, protect your credit with debt-validation rights and by avoiding statute-of-limitations pitfalls. Most of all, keep everything in writing and escalate calmly when rules aren’t being followed. Put today’s guide into action on your current bill, and save this workflow—your future self will thank you. Ready to start? Request the itemized bill and EOB today, then send a written, anchored offer this week.
References
- Medical Bill Rights (Consumer Pages) — CMS, updated Nov 5, 2024. CMS
- No Surprises Act Overview of Rules & Fact Sheets — CMS, updated Aug 11, 2025. CMS
- No Surprise Billing (Consumer & Compliance Hub) — CMS, updated Apr 23, 2025. CMS
- Dispute a Medical Bill (PPDR, $400 Threshold) — CMS, updated May 19, 2025. CMS
- What Is a Good Faith Estimate? (GFE Guide) — CMS, updated Nov 5, 2024. CMS
- Hospital Price Transparency (Overview) — CMS, updated May 22, 2025. CMS
- Hospital Price Transparency – 2024/2025 Requirements (Webinar Slides) — CMS, Oct 21, 2024 (PDF). CMS
- Explanation of Benefits (EOB) — Consumer Guide — CMS, updated Nov 5, 2024. CMS
- IRS Section 501(r)(4): Financial Assistance Policy; 501(r)(5) Limitation on Charges; 501(r)(6) Billing & Collections — IRS, updated Jul 1–2, 2025. ; https://www.irs.gov/charities-non-profits/limitation-on-charges-section-501r5 ; https://www.irs.gov/charities-non-profits/billing-and-collections-section-501r6 IRS
- Physician Fee Schedule Look-Up Tool — CMS, updated Jun 19, 2025. CMS
- FAIR Health Consumer (Cost Lookup Tool) — FAIR Health, accessed 2025. fairhealthconsumer.org
- Health Care Debt in the U.S. (KFF Survey) — KFF, Jun 16, 2022; updated summaries Jul 11 & Jul 23, 2025. ; https://www.kff.org/health-costs/americans-challenges-with-health-care-costs/ ; https://www.kff.org/quick-take/polling-on-medical-debt-illustrates-the-challenges-that-blocked-credit-reporting-rule-sought-to-address/ KFF
- Equifax, Experian & TransUnion Remove Medical Collections < $500 — TransUnion Newsroom, Apr 11, 2023. TransUnion Newsroom
- CFPB Final Rule on Medical Debt in Credit Reports (and Litigation Status) — CFPB Newsroom, Jan 7, 2025; AP News follow-up on court action, Aug 2025. ; https://apnews.com/article/41f212ee6b89f9902deb267d75ab8443 Consumer Financial Protection Bureau
- Debt Collection Rights: Validation Notice & 30-Day Dispute Window — CFPB Ask-CFPB, updated Sep 10, 2024; Regulation F §1006.34. ; https://www.consumerfinance.gov/rules-policy/regulations/1006/34 Consumer Financial Protection Bureau
- Regulation F: Time-Barred Debt (No Suits or Threats to Sue) — CFPB Advisory Opinion & Federal Register, May 1, 2023. ; https://files.consumerfinance.gov/f/documents/cfpb_regulation-f-time-barred-debt_advisory-opinion_2023-04.pdf Federal Register
- Patient Advocate Foundation (Case Management & Financial Aid Funds) — PAF, accessed 2025. ; https://copays.org/ Patient Advocate Foundation
- Undue Medical Debt (Program & Public Partnerships) — Undue Medical Debt; Reuters/AP coverage of state/local relief, 2024–2025. ; https://www.reuters.com/world/us/new-jersey-governor-phil-murphy-forgives-100-mln-medical-debt-2024-08-20/ ; https://www.axios.com/local/cleveland/2025/05/05/cleveland-erases-medical-debt-residents ; https://apnews.com/article/708b61e795cbb2b05cf6b2647de6927c AP NewsUndue Medical DebtReuters