If you’ve ever wondered whether you need an advance healthcare directive, a living will, or both, you’re in the right place. The short answer: a living will records your treatment preferences for serious medical situations, while an advance healthcare directive (often just called an advance directive) is a broader document that can also appoint someone to make decisions for you if you can’t speak for yourself. Put simply, a living will tells people what you want; an advance directive can add who decides.
Before we go further, a quick note: this guide is for general education and planning. Health laws and forms vary by state and personal circumstances. For decisions with legal or medical consequences, talk with a licensed attorney and your clinicians.
Skimmable plan:
- Choose a trusted healthcare agent (decision-maker).
- Write down your treatment preferences (living will section).
- Sign the document correctly (witnesses or notary, per your state).
- Share copies with your agent, family, and clinicians; add to your medical record.
- Review after major life events or changes in health.
When you’re done reading, you’ll know exactly how these documents differ, when each one applies, how to make them valid in your state, and how to keep them useful in real life.
1. Definitions That Actually Matter
A living will is a legal document stating your preferences for specific medical treatments if you cannot communicate—think resuscitation, ventilators, feeding tubes, and the like. An advance healthcare directive is an umbrella term: it can include a living will and let you designate an agent (also called a proxy) to decide for you when you’re incapacitated. This distinction matters because life is messy; even the best checklist can’t predict every clinical twist, but an agent can interpret your values in the moment. Authoritative health sources draw the same line: written treatment instructions (living will) and broader planning (advance directives), often with the option to appoint an agent.
Why it matters
- Predictability vs flexibility: A living will is precise about scenarios; an advance directive adds a human decision-maker for gray areas.
- Care team usability: Clinicians use both to guide care when you can’t express choices.
- Legal footing: Most states recognize both forms; terminology varies.
Numbers & guardrails
- Expect two core parts in a comprehensive advance directive: (1) agent appointment (medical power of attorney/health care proxy) and (2) treatment instructions (living will). Many official templates are structured exactly this way.
Bottom line: Use a living will to document your preferences and an advance directive to pair those preferences with a trusted decision-maker.
2. Scope: What Each Document Actually Covers
At the simplest level, a living will addresses the treatments you would accept or decline in serious illness or near end-of-life situations when you can’t speak. Common topics include CPR (cardiopulmonary resuscitation), intubation and mechanical ventilation, dialysis, antibiotics, and artificial nutrition/hydration. An advance healthcare directive may contain the same instructions plus broader guidance about your values, goals, and quality-of-life tradeoffs, and it can name an agent to decide in unforeseen situations. Clinically, the goal is to translate your values into care plans your team can follow quickly and confidently.
How to do it
- State preferences plainly: “If I can’t recognize loved ones or live independently, I would decline X.”
- Prioritize outcomes, not only treatments: “Comfort over longevity” or “Try full treatment for two weeks; if no improvement, shift to comfort.”
- Include values: Pain control, religious considerations, and where you prefer to receive care.
- Add exceptions: For example, “Attempt a time-limited trial of ventilation if short-term recovery is likely.”
- Document organ donation wishes in the directive if desired.
Common mistakes
- Listing only “yes/no” without context.
- Forgetting antibiotics or dialysis.
- Skipping preferences about artificial nutrition/hydration, a frequent source of conflict.
Synthesis: Spell out the care you want and when; give your agent flexibility to honor your values when reality doesn’t match the form.
3. Your Healthcare Agent: The Most Powerful Choice
Naming a healthcare agent (also called a health care proxy or surrogate) turns your plan from a static list into a living decision process. The agent can talk with physicians, review options, and make choices consistent with your values when you can’t. This authority is typically created in the medical power of attorney section of an advance directive and is distinct from financial power of attorney. Model laws and professional groups describe agent appointment as a core element of modern directives.
Why it matters
- Continuity: An agent handles unexpected scenarios your living will didn’t imagine.
- Clarity: Clinicians have a single, authorized voice to consult.
- Legal access: A properly authorized agent is usually treated as your personal representative under HIPAA, with rights to relevant medical information.
Numbers & guardrails
- Name one primary agent and at least one alternate.
- Make sure your agent knows your values and is comfortable advocating for you; distribute identical copies to all alternates.
- Use state-compliant forms and signature rules to avoid disputes.
Synthesis: If you do only one thing, choose and brief a capable agent—this single decision resolves most gray areas with compassion and legality.
4. When Each Document “Turns On”
Neither a living will nor an advance directive replaces your voice while you can make decisions. They generally take effect when you lack capacity to make or communicate choices. A living will usually applies in circumstances like terminal illness, permanent unconsciousness, or advanced dementia with inability to express preferences. An advance directive with an agent allows that agent to decide any time you’re deemed unable to make health decisions—temporarily (e.g., sedation) or longer term—within the bounds of your instructions and state law. Health systems and clinicians rely on these triggers to follow your plan ethically.
Numbers & guardrails
- Expect capacity determinations to be made clinically; some forms require one or two clinician certifications before the agent’s powers activate.
- In many states, your agent’s authority ends when you regain capacity—your voice takes over again. (Exact standards vary; use state forms.)
Mini case
You’re intubated for a severe pneumonia and sedated. Your directive names a proxy and says, “Prioritize recovery with a two-week trial of full support; if no meaningful improvement, focus on comfort.” Your agent confers daily with the ICU team; on day 10, progress is strong, so treatment continues. The document’s trigger and time-limited trial make decisions clear.
Synthesis: Directives activate only when you can’t decide; write them to guide both short-term crises and long-term conditions.
5. State Rules: Witnesses, Notaries, and Portability
Advance directive requirements are state-specific. Some states require two witnesses, some allow notarization instead, and a few require both for certain choices. Many reputable organizations publish free, state-specific forms and instructions that lay out the exact signing rules and who may serve as a witness. Because requirements vary—and can differ for out-of-hospital orders and mental health directives—using your state’s official or vetted form is the safest route.
Region-specific notes
- Witnessing vs notarization: For example, some states let you either have two adult witnesses or use a notary; others specify only one option. The instructions embedded in state forms spell this out. CaringInfo
- Interstate portability: States often honor out-of-state directives that meet either their law or the originating state’s law, but not all treat them the same; completing directives for every state where you spend significant time is a conservative approach.
Numbers & guardrails
- Use your state’s form, sign it exactly as directed, and distribute at least five copies: you, your agent(s), your primary care clinic, your hospital system, and a trusted family member.
- If you split time across states, keep state-specific versions in the places you receive care.
Synthesis: Validity depends on state rules; follow the form, sign it right, and keep versions where you actually get care.
6. Treatments You’ll Be Asked About (CPR, Ventilation, Feeding Tubes & More)
Living wills commonly address whether to attempt CPR, use mechanical ventilation, start dialysis, continue antibiotics, or provide artificial nutrition and hydration (ANH). Your choices can be nuanced: many forms allow time-limited trials (e.g., “try ventilation for up to two weeks”). Be specific about comfort measures, pain control, and situations where you would accept treatment for recovery but not continued life support with low chance of meaningful function. Medical references emphasize these as standard categories in advance care planning.
Tools/Examples
- Use reputable templates that list these interventions clearly; many hospital and nonprofit forms include “Yes/No/Trial period” options and space for values statements.
- Distinguish DNR/DNI (do-not-resuscitate / do-not-intubate orders) from your directive; DNR/DNI are medical orders written by a clinician for current care settings, while your directive is a legal instruction for future scenarios. For seriously ill people, POLST forms translate preferences into portable medical orders that first responders honor.
Numbers & guardrails
- Consider three tiers for each treatment: accept, decline, or trial period with criteria for stopping.
- Ask your clinician about likely outcomes; for example, CPR success rates in frail patients are typically low, which may influence your choices.
Synthesis: Get concrete about which treatments you’d want under which conditions; clarity here prevents the hardest bedside conflicts.
7. HIPAA, Privacy, and Who Can See Your Directive
For your plan to work, your decision-maker and clinicians must access your information and your document. Under federal privacy rules, a properly authorized personal representative generally “stands in your shoes,” meaning covered entities must treat them as you for purposes of access relevant to their role. That access allows an agent to request records, discuss prognosis, and coordinate care. Practically, you should provide your agent with copies of your directive and make sure your healthcare providers have it on file.
How to do it
- Give your agent paper and digital copies; store a PDF in shared cloud storage.
- Ask your primary care clinic to scan it into your electronic health record (EHR) and confirm it’s visible in the “Advance Directives” section.
- Carry a wallet card noting you have an advance directive and who your agent is.
Mini-checklist
- Agent and alternate named
- Copies to agent, alternates, and key family
- Uploaded to clinic/hospital EHR
- Wallet card or phone lock-screen note
Synthesis: Access unlocks your plan; combine legal authority with practical sharing so the right people can act quickly.
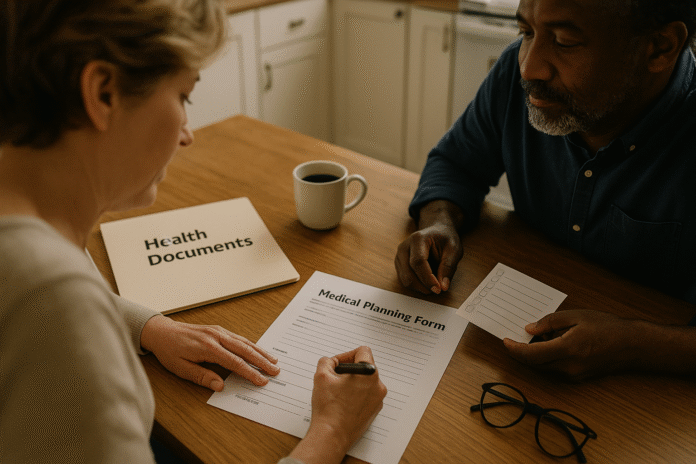
8. How to Create, Sign, and Store It (Without Overthinking)
You don’t need to reinvent the wheel. Start with a state-specific template from a reputable organization, follow its instructions to the letter, and sign with the required witnesses and/or notary. Then distribute copies and note the location for loved ones. Many forms include space for organ donation, spiritual preferences, and physician contact details. A simple, complete process beats a perfect but unfinished plan.
Numbers & guardrails
- Budget 30–60 minutes to complete, 10–15 minutes to sign correctly, and 15 minutes to share and upload.
- Keep two originals (one at home, one with your agent).
- Revisit after major life events (marriage/divorce, diagnosis, relocation).
Mini case
You download your state’s packet, appoint a partner as agent and a sibling as alternate, and choose a “trial period” for ventilation. You sign with two independent witnesses (not agents or healthcare staff), scan the final document, upload it to your clinic portal, and email it to your agent. The clinic confirms it’s in your EHR’s “Advance Directives” tab. That’s a fully executed plan in under two hours.
Synthesis: Use official forms, follow the signing rules precisely, and make sure finished documents land where clinicians can find them.
9. Updating, Revoking, and Avoiding Conflicts
Your preferences can change—and so can the law. You can usually revoke a directive by destroying it, creating a new one, or telling your clinician and agent. The key is to replace copies everywhere the old version lives and inform everyone who relied on it. Many people revisit directives after a major diagnosis, a change in relationships, or a move. Organizations that publish state forms encourage periodic reviews and clear revocation steps.
Common pitfalls
- Leaving multiple versions in circulation.
- Not telling your agent about changes.
- Moving states without updating the form.
- Forgetting to switch documents in your EHR.
Numbers & guardrails
- Do a review every couple of years or after major life events; if you revise, distribute all-new copies the same day.
- Keep a version date in the filename (e.g., “Advance-Directive-Jones-v3.pdf”) so everyone knows the latest copy.
Synthesis: Your directive is living; update intentionally and replace old versions everywhere to avoid confusion at the bedside.
10. Special Cases: POLST, DNR/DNI, Pregnancy, and Mental Health
Some situations call for additional documents. POLST (or similarly named programs like MOLST, POST, MOST) are medical orders for people who are seriously ill or frail; they complement but do not replace an advance directive. DNR/DNI orders are signed by a clinician and tell teams not to attempt CPR or intubation; these can exist in the hospital or at home (with state-specific out-of-hospital forms). Pregnancy can change how states apply directives; several states limit or invalidate a pregnant person’s living will. Psychiatric advance directives (PADs) let you state preferences for mental health treatment and name a decision-maker for behavioral health crises.
Region-specific notes
- POLST vs advance directive: POLST is a doctor-signed order set that first responders follow; advance directives are legal documents for future decisions and agent appointment. Use POLST when serious illness or frailty makes near-term decisions likely.
- Pregnancy exclusions: Some states restrict or invalidate directives during pregnancy; check your state’s rules and discuss with your clinician.
- Mental health: PADs are recognized in many jurisdictions and supported by national behavioral health agencies as tools for autonomy in crises.
Synthesis: Match the tool to the situation: advance directive plus agent for broad planning, POLST or DNR/DNI for current medical orders, and PADs for behavioral health scenarios.
11. Getting Everyone on the Same Page (Clinicians & Family)
Even the best form can falter without conversations. Tell your agent why you chose them, explain your values, and walk through common scenarios so they aren’t surprised. Ask your clinician, “If I had a sudden stroke tomorrow, how would this directive guide you?” Share copies with family to reduce conflict and appoint an alternate who can step in seamlessly. Most disagreements arise not from malice but from uncertainty—conversations eliminate guesswork.
Mini-checklist (conversation)
- Share your values and outcomes that matter most
- Clarify “try, then stop” time limits for intensive treatments
- Discuss organ donation and comfort care
- Confirm your agent is comfortable speaking up
- Tell your clinician where the directive is stored
Tools/Examples
- Many health systems provide conversation guides alongside forms; your agent can attend a clinic visit to document preferences in the chart. Vetted state packets typically include talking points and wallet cards.
Synthesis: Conversations transform a document into a plan your loved ones and clinicians can carry out with confidence and unity.
Quick Comparison Table
| Feature | Advance Healthcare Directive | Living Will |
|---|---|---|
| Primary purpose | Broad plan; may appoint an agent and include treatment preferences | Specific treatment preferences |
| Includes decision-maker? | Yes (medical power of attorney/proxy) | No (instructions only) |
| When it applies | When you lack capacity, across scenarios | Typically terminal illness, permanent unconsciousness, or similar |
| Legal vs medical | Legal document; guides clinical care | Legal document; guides clinical care |
| Becomes medical orders? | No—can inform orders | No—can inform orders |
| Who signs | You + witnesses/notary per state | You + witnesses/notary per state |
| Good companion | POLST (if seriously ill/frail), DNR/DNI orders | POLST (if seriously ill/frail), DNR/DNI orders |
References for distinctions and usage across this table are drawn from major medical and legal sources.
FAQs
What’s the simplest way to decide between a living will and an advance directive?
You don’t need to choose—use an advance directive that includes a living will section. That gives you written preferences and an agent to interpret them. Most state packets bundle both parts.
Do I still need a POLST if I have an advance directive?
Only if you’re seriously ill or frail and want your choices translated into medical orders that emergency teams follow. POLST complements, not replaces, your directive. If you’re generally healthy, a directive is usually sufficient.
Is a living will valid if I’m traveling to another state?
Often yes, but rules differ. Many states honor out-of-state directives; to be safe, complete forms for states where you spend significant time and keep copies with you and in your medical record.
Who can I pick as my healthcare agent?
Choose a calm, assertive adult who understands your values and will advocate for you. Most states bar your treating clinician or facility staff from serving. Name an alternate. Provide them access rights and copies.
Do I need witnesses or a notary?
Yes—almost always one or the other, sometimes specific to your state. Your state’s instructions will list who can serve as a witness and whether notarization is allowed or required. Follow those rules exactly.
How do DNR/DNI orders relate to my living will?
Your living will expresses preferences; a DNR/DNI is a clinician’s order. In the hospital, a DNR/DNI can be written to match your wishes. At home, some states have portable DNR forms for EMS.
What about pregnancy—can that limit my directive?
In several states, pregnancy laws can restrict or invalidate a person’s directive. If pregnancy is possible for you, ask your clinician and consider state counsel to understand specific implications. FindLaw
Are there directives for mental health care?
Yes—psychiatric advance directives (PADs) let you state preferences and appoint a decision-maker for behavioral health crises. Many public health agencies support them as tools for autonomy. library.samhsa.gov
Can my family override my directive?
Legally, clinicians should follow your valid directive and your authorized agent. Disputes arise when documents are missing or unclear; conversations and exact state compliance reduce the risk dramatically.
How often should I update my documents?
Review after major life events or health changes, and update sooner if your preferences evolve. Replace all old copies and upload the new version to your medical record each time. CaringInfo
Conclusion
Clear, compassionate care starts long before a crisis. A living will captures the treatments you would accept or decline; an advance healthcare directive adds the power of a trusted agent who can apply your values when facts are messy. Together, they spare your loved ones from agonizing guesswork and give clinicians the clarity they need to do the right thing. The process is straightforward: pick your agent, write down preferences with honest “if/then”s and time-limited trials, sign exactly as your state requires, and then share, upload, and revisit as life changes. With that, you’ve turned uncertainty into a plan your future self will thank you for—and your loved ones will feel confident carrying out.
Ready to act? Download your state’s forms, choose an agent, and finish your directive this week—so your care always reflects your voice.
References
- Advance Care Planning: Advance Directives for Health Care, National Institute on Aging, publication page. National Institute on Aging
- Living wills and advance directives for medical decisions, Mayo Clinic. Mayo Clinic
- Guidance: Personal Representatives, U.S. Department of Health and Human Services, Office for Civil Rights (HIPAA). HHS.gov
- POLST & Advance Directives, National POLST. POLST
- Portable Medical Orders (POLSTs) vs Advance Directives, CaringInfo (National Hospice and Palliative Care Organization). CaringInfo
- Download and Complete Your State or Territories’ Advance Directive Form, CaringInfo—state-by-state packets and signing rules. CaringInfo
- Health Care Decision Making, American Bar Association Commission on Law and Aging—resources and model guidance. American Bar Association
- Current Acts – Health Care Decisions Act, Uniform Law Commission. uniformlaws.org
- DeMartino ES, US State Regulation of Decisions for Pregnant Women, Journal of the American Medical Association Network Open (via PubMed Central). PMC
- A Practical Guide to Psychiatric Advance Directives, Substance Abuse and Mental Health Services Administration. SAMHSA
- An Advance Health Care Directive (form packet), Mayo Clinic (patient form). https://mcforms.mayo.edu/mc2100-mc2199/mc2107-07.pdf mcforms.mayo.edu
- Advance Directives—What Are They and When Should You Create One?, National Council on Aging. ncoa.org